This was not a good way to start off the week. Woods was scheduled to start a summer class and was supposed to take a physical for a second job driving a bus that would, with luck, see her through the next several months. Because she would be laid off from her regular job, driving a school bus, until September, she needed the extra income until starting back in fall.
The fact that her ex-husband had lost his job at Boeing didn't help matters much. The child-support payments were virtually nonexistent these days, so, between that and her summer break from work, Woods decided to apply for Medicaid. It was just a backup plan, in case she didn't get the summer job, but she wasn't too worried, because she had never had trouble getting work before.
And it wasn't as if she was asking for cash assistance. She didn't want any handouts. She'd get a job flipping burgers if she had to, but there wasn't a minimum-wage job out there that would pay for her family's health insurance, and there were the three kids -- Tamia, 9; Damien, 11; and Stephen, 15 -- to think about, after all.
Applying for Medicaid was no easy matter for Woods. There were offices to find, lines to stand in, forms to fill out. She had to provide this, verify that, calculate these and double check those. Was she in income bracket A, B or C? Were her assets closer to D, E or F? Sign here, please. Thank you. And here. Thank you. And here. Thank you. She felt trapped in a maze of dotted lines.
It bothered Woods that she didn't understand any of it. All she knew was what her caseworker told her -- that she would be enrolled in one category of Medicaid and her children would be enrolled in another. Woods didn't try assessing the ins and outs of the coverage -- wished, in fact, that she didn't have to deal with any of this at all -- she had no insurance from her regular job driving a bus, so she had to stand in line.
But several weeks after Woods was approved to receive Medicaid, as she held her aching jaw in one hand and the telephone in the other, she was informed by her caseworker that dental care wasn't covered by the category of Medicaid she was enrolled in.
"I really didn't understand what was going on," Woods says. "I found out later that I had like four abscessed teeth, but all I knew was that I was in a lot of pain, and they were telling me to call another number. I didn't know what this other number was, but I called it."
The woman who picked up the phone was a social worker for something called the MC+ Consumer Advocacy Project. But Woods didn't know what this place was or why she was supposed to call. Frankly, she didn't care. If they could help cure the misery in her mouth, that was all that mattered. She could hardly stand the pain.
Five days went by, and the social worker called her back to tell her that Woods' caseworker had incorrectly placed her in the wrong category of Medicaid. The social worker, a nice woman who apologized a lot, said that she had called the Missouri Department of Social Services (DSS) over and over again but had just gotten word back from them that day. The social worker went on and on about things that Woods didn't quite understand -- stuff about "transitional Medicaid" and "MC+" and "time limits" -- and all Woods could think about was getting to a dentist. She couldn't eat or drink anything, and she'd already missed the physical she was supposed to take for her new job.
The social worker told Woods her category would be changed but that it would take a couple of weeks, so in the meantime she would be enrolled in yet another category. Then the social worker gave Woods the names of three oral surgeons from a list supplied to her by DSS. Woods immediately contacted all three, but none of them accepted patients in the category of Medicaid that she was enrolled in.
Woods phoned the social worker and was given the names of six more oral surgeons from the DSS list. When Woods contacted them, one had retired, four didn't accept clients in her Medicaid category and the sixth would take her only if she paid $160 up front for the anesthesia. As far as Woods was concerned, $160 could have been $1 million. She simply didn't have it.
So Woods called back the social worker, who said she'd try to find an oral surgeon. Three days later, the social worker got back to Woods with still more bad news: She had asked DSS for the names of oral surgeons in Jefferson, Franklin and St. Charles counties, but there was none in Jefferson and Franklin counties, and the only one in St. Charles wasn't accepting any more Medicaid clients, no matter what category they were in. The social worker told Woods that she would try to get her into the new category as soon as possible.
The next day, Woods got the first good news in more than two weeks: A DSS supervisor told the social worker that Woods would be enrolled in the new Medicaid category in three days, which meant that she wouldn't have to contend with oral surgeons who didn't accept her current category.
But three days could have been an eternity, for all Woods' mouth was telling her. She had already lost the summer job, so she was getting behind in the bills, and because she hadn't eaten anything -- she was living on water and rolled-up pieces of bread -- she was losing weight. Meanwhile, her kids were doing all of the cooking and cleaning. Two of them also had doctors' appointments scheduled for the next week, and Woods prayed that her teeth would be taken care of by then so they could make it.
Four days later -- and almost three weeks after being told by her DSS caseworker that she wasn't covered for dental work -- Woods was enrolled in her new category and on her way to an oral surgeon, who pulled two of her teeth. Two other teeth were still abscessed, though, and wouldn't be pulled until Friday. Why, she wasn't told.
In the meantime, Woods learned that two of her children weren't enrolled in the Medicaid categories they were supposed to be in either, because, according to the social worker, the caseworker who changed Woods' category of Medicaid after making a mistake on the first category of Medicaid made another mistake and changed her kids' category as well. It was a big mess-up that had something to do with computers and a new system and the caseworkers' not understanding the system very well. The kids were still covered, the social worker said, but it was a different category, and they needed to show the doctors a different kind of Medicaid card.
"Why didn't they tell me that?" Woods asked.
"Who knows?" the social worker replied.
That Friday, after having spent three weeks nearly mad with pain, Woods went back to the oral surgeon at 9 a.m. Finally, she thought, it would all be over. But there was a problem, the receptionist told Woods. For some reason, the health-care plan of her new Medicaid category wouldn't authorize the second surgery.
It had now been almost three weeks since she woke up with the pain in her mouth, and all Woods could think was "Do I have to go through this all again?"
Woods phoned the social worker from the dentist's office and told her what was happening.
"Hold that thought," the social worker said. "I'll get back to you as soon as I can."
Woods waited three hours in the office for the call. But by the time the social worker got approval from the health-care plan, the dentist had left for the day.
Woods' teeth were pulled on Saturday, but her relief was only physical.
She had not gotten a summer job. She was not enrolled in school. She was negotiating with the landlord about paying her rent, and her telephone was going to be cut off. Less than a month after her teeth were pulled, Woods was not only on Medicaid and food stamps, she was also waiting for a cash grant from welfare. It was money she had hoped she would never have to ask for, but the phone company was sending threatening disconnection notices.
That week, when she went to an ATM to withdraw the cash using a state-issued electronic-benefit-transfer (EBT) card, the machine sucked the card in and never spit it -- or the money -- back out.
Woods immediately dialed the emergency number in Wisconsin but was still waiting for a new card one week later. In the meantime, her phone was disconnected and the family began to run low on food. Woods had a job interview lined up, but there was no gas in the car to get there. As she scoured the apartment for loose change, her 11-year-old son offered up a $10 bill someone had sent him for his birthday.
"He told me I should take it," she says with tired irony.
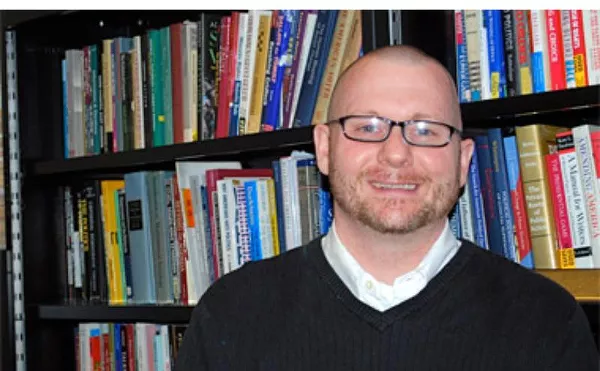
When the phone rang in Cathy Goldstein's office last July, she knew it wouldn't be good news. It never was, especially since federal welfare-reform laws had kicked in two years earlier, the Medicaid program was expanded and the state tried fashioning policies around both. Goldstein was a social worker and director of the MC+ Consumer Advocacy Project, which meant she was supposed to help people in St. Louis who were having trouble with their Medicaid coverage.
On her desk lay a mass of folders, each representing a client with complex, convoluted, time-consuming problems. Each folder was fat with the bureaucratic essentials -- applications, waivers and verification forms -- and each demanded resources she couldn't find or couldn't find time to look for.
And then there was the phone. Ever since February 1999, when the state expanded its Medicaid program to children in working families earning up to 300 percent of the poverty level, it never stopped ringing. She had multiple lines, and at the moment they were ringing in unison. Every call, Goldstein knew, was someone who desperately needed help getting health care, and every call represented what went wrong when the government answered the public's demand to provide it.
When Goldstein picked up the phone and heard Fayzen Woods explain that she was in pain, couldn't go to a dentist, didn't understand why and didn't know what to do, the social worker knew another fat file was headed for the towering stack on her desk.
It was a clash in philosophies, really, that was creating this mess. When Congressional conservatives pushed "welfare reform" and President Bill Clinton signed the Personal Responsibility and Work Opportunity Reconciliation Act back in 1996, they placed limits on the amount of time citizens could receive public aid. At the same time, affordable health insurance was becoming such a scarce commodity for so many Americans, Congress allowed the states to use money they saved cutting welfare to expand Medicaid health insurance for the poor.
The results were new laws and regulations that read like a dissertation on post-World War II particle physics. Goldstein was a social worker with years of experience, but she felt overwhelmed. None of the people calling her had a clue about how to traverse the system, and, judging from the sheer number of calls referred to her by DSS caseworkers, the caseworkers didn't, either.
"It's all so complicated," Goldstein says now, throwing her hands in the air. "We're getting so many referrals from caseworkers who should know how to resolve these problems but can't because the system is so complicated. It's not a criticism of the caseworkers, really. I mean, these are never-ending cases, and one little glitch sets it all off."
Goldstein knew it was not a situation unique to Missouri, either. Across the country, state social-service agencies were madly trying to plug policy holes. But they were in every nook and cranny of the law. According to a report issued in March by Covering Kids, a national organization funded by the Robert Wood Johnson Foundation, the Medicaid system was grinding to a slow halt under new rules piled on old rules that were too complicated to begin with.
"The complicated eligibility rules and regulations for children's Medicaid coverage ... thwart efforts and efficiency, deplete the energy of overburdened eligibility staff and significantly restrict the ability of community organizations to be effective in helping families enroll their children," the report states.
Goldstein knew this all too well. Since February 1999, the vast number of calls coming in had forced her to close the project to new clients on several occasions. There were just too many files on her desk already. There was the mother of two children who lost Medicaid because she missed a meeting with her caseworker that she hadn't been notified about. There was the 12-year-old foster child, accused of molesting other children and eating kittens alive, who couldn't get psychiatric counseling because the juvenile court couldn't figure out how to navigate his Medicaid category. There was the woman who couldn't figure out how to get dental care through her Medicaid program and ended up, in the messy bureaucratic end, losing all of her teeth.
"Try getting a decent job with no teeth," Goldstein says. "The system is so complicated, there is no way people, including caseworkers, can get it right. They aren't trained well enough, and there aren't enough of them. The fact that it ever gets done right is a miracle."
The real miracle, as far as Goldstein is concerned, was just getting someone from DSS to return her call about Fayzen Woods. When she first tried to change Woods' Medicaid category so that the woman could receive dental care, she dialed the numbers of four different people at DSS. Of those four, only one called her back, and that took five days. Goldstein apologized to Woods about the delay, but how do you explain to someone in extreme pain over an extended period of time that government office workers don't answer their phones and don't have answering machines?
Then there was the ordeal of finding an oral surgeon who accepted Medicaid fee-for-service clients. In a five-county region, there was only one, and he required an up-front fee that most Medicaid recipients couldn't afford.
When Goldstein contacted the office of the director of DSS in Jefferson City to complain about the lack of providers, she was told that if Woods could find a new oral surgeon willing to accept Medicaid clients, their office would walk the surgeon through the process of getting signed up. "If it was that easy," an outraged Goldstein responded, "we wouldn't be in this situation right now."
In desperation, she dialed Gov. Mel Carnahan's office and left a message with a staffer: Her client needed help. It was a desperate situation. No one at DSS seemed able to deal with the problem. She was never called back.
Finally Goldstein got a break. A DSS caseworker called to say that Woods would be enrolled in a managed-care program in her new Medicaid category in three days. That meant she wouldn't have to contend with trying to find an oral surgeon who would accept fee-for-service patients. Goldstein immediately contacted the managed-care plan so that she could make an appointment with one of its oral surgeons. She left a message but wasn't called back for another three days. The representative from the plan who finally got back to her said not to worry, she'd already made an appointment for Woods.
"Great," Goldstein said. "When?"
"Today," the representative said.
Goldstein asked what time the appointment was, and the representative answered that it was scheduled for 10 a.m.
Goldstein looked at her watch. It was noon.
Apparently the representative from the plan had made the appointment but never called Woods or Goldstein to tell them. After apologizing, the representative promised to schedule another appointment for the next day, took Woods' number and promised that she would contact Woods and tell her about it.
You do that, Goldstein said.
The next day, the phone rang again. It was Woods, this time at the oral surgeon's office waiting to have her last two abscessed teeth pulled. The health-care plan, however, wouldn't authorize the surgery.
Goldstein immediately phoned the health-care plan but was put on hold for 20 minutes. Then she was disconnected.
Goldstein was frantic. It was now late July; Woods had already gone three weeks with four abscessed teeth; and, because this was Friday, there was a good chance she'd have to go yet another weekend in pain. Goldstein dialed the health-care plan again and asked for a woman she knew who worked not with dental-care issues but with mental-health care.
"I was calling anybody, just to get a name," Goldstein says. "And I explained to this woman that I knew this case had to do with teeth but, quite frankly, was going to evolve into a mental-health problem pretty soon."
Goldstein's client eventually got all of her bad teeth pulled, but by that time she had lost a job, missed out on summer school, had her phone cut off and had gone on welfare.
"Here was a woman who could have been a productive, tax-paying citizen. She just needed a little help, and look where she ended up," Goldstein says.
"And this sort of thing happens all the time."
The expansion of Medicaid by Congress was called the Children's Health Insurance Program (CHIP), and it allowed states to cover the children of working parents who didn't earn enough money to buy private health insurance but earned too much to qualify for traditional Medicaid.
When Congress allowed the states to expand their Medicaid programs, some 23 million children were on traditional Medicaid and another 10 million were expected to come into the new CHIP program. At the time, almost 9 percent of the children living in Missouri had no Medicaid or private health insurance, so the state Legislature opted for CHIP and invited children in families earning up to $41,640 -- or 300 percent of the federal poverty level -- into the new program.
Conservatives in the state Legislature, however, choked on the idea of unfurling Medicaid to cover more people: It was welfare, plain and simple. They demanded some limits and piled on a torturously long list of name changes, program limitations and undefinable and forever unfolding do's and don'ts. For example, they erected a maze of income hedgerows within the expanded Medicaid program that required sheer physical stamina to traverse. There were gross-income, net-income and no-income standards, each with its own subset of co-payments, premiums and benefits. A single mother with a specified number of children making a specified amount of money who had private insurance didn't qualify, but another single mother with the same number of children, making the same amount of money, who didn't have insurance for a specified amount of time did. Maybe some of the kids did, though. Maybe they didn't.
"The legislators were looking to save money for the state, but what they ended up creating is this extremely complicated program that no one, from the (DSS) supervisors on down, has a handle on," says Monique Paulson, spokeswoman for the Missouri State Workers Union Local 6355, the elected bargaining representative for more than 7,000 DSS employees.
So at the same time the state was supposed to wean some 283,000 people from welfare, it was also supposed to bring in an estimated 91,000 children eligible for the expanded Medicaid benefits. This meant that DSS, like its counterparts in every other state, had to not only gut and rebuild its public-aid program but expand and remodel it at the same time.
According to a report recently released by the Urban Institute, titled "The Medicaid Eligibility Maze," policy changes by federal and state governments created a system so complex that no one, at any level, has a firm grasp of it all. "Though well intentioned," the report states, "these rules create barriers to program participation by making the eligibility process difficult for Medicaid applicants and beneficiaries, as well as staff, to understand."
So many changes were happening so quickly that DSS began issuing hundreds of memos to its employees in an effort to explain what was going on. In August 1999 alone, for example, 21 memos updating employees about the ever-evolving changes were issued with such memorable titles as "Forms Manual Revision #32; FPAY Instructions, FSU5 Instructions, Appendix E, Pages 1-3" and "MC+/MAF Income Verification Requirements Forms Manual Revision #30: Im-1UA, MC+ Application; IM-31A(MC+), MC+ Request for Information."
One caseworker in St. Louis County, who asked not to be named, has enough filed memos regarding all of the changes to wallpaper her house. "We have to know about food stamps and welfare and Medicaid, each with totally different eligibility rules and each with totally different benefits," the caseworker says, adding that a caseworker might have 350 families in his or her care who may or may not be eligible for programs including food stamps, welfare and Medicaid.
"There are more ins and outs, ups and downs, and right triangles than I really want to think about," she says. "They've made it so complicated, a lot of us don't have a clue about all the different programs."
The first load of new rules came down with welfare reform and required, for example, that every food-stamp recipient reapply for benefits every three months. This meant that each client had to fill out -- and each caseworker had to process -- a two-page application, a work form, a two-page worksheet and an employment-verification form every 90 days for every recipient.
And that was just one food-stamp requirement. But then the state Legislature expanded Medicaid and ushered in a whole new, much more complicated, set of rules. The expanded program, for instance, fell under the name "MC+." But 17 other categories of the state's Medicaid coverage also congregated under the name "MC+." Each category had a different name, different income requirements and different coverage. They included such categories as "Medical Assistance for Families," "Transitional Medical Assistance," "Extended Transitional Assistance" and "Extended Medical Assistance for Families for Support Related Closings." There was an MC+ for Pregnant Women, an MC+ for Newborns and six categories of MC+ For Children, depending on which subcategory the child was in: Non-CHIP, CHIP No Cost Sharing, CHIP Co-Pay or CHIP Premium.
"We are totally overwhelmed," the caseworker says. "I mean, when the MC+ program expanded, it exposed us to a whole new set of clients that we never had before. Believe me, they ran into a lot of crabby caseworkers who were trying to process 10 applications a day, trying to work with computers that don't work, trying to understand all the new rules."
Until this month, caseworkers didn't even have voice mail. "If someone called me for help and I wasn't at the desk, that person didn't get any help," the caseworker says.
In addition to what the caseworkers had to grapple with, providers such as physicians and pharmacists had to contend with a blizzard of special bulletins keeping them up to date on all of the changes: "...the medicaid Maximum Allowed Amount for procedure code 99211 equals $5.00; therefore, the provider should charge the recipient with ME code 74 a $5.00 co-pay. The provider should only charge $5.00 to recipients with ME codes 75, 76, 77 and 79 instead of $10 because the Medicaid maximum Allowed Amount is less than the co-pay amount of $10.00."
That bulletin, from last November, contained two pages of similar clarifications and was followed by one page of corrections for mistakes made in earlier bulletins: "Special Bulletin Vol. 21, No. 4 dated January 22, 1999, page 7 shows provider types 33 and 34 must charge a co-pay for ME codes 76, 77 and 79 for procedures using code 92506. This is incorrect. The procedure is covered as an HCY service only. Uninsured working parents are not eligible for the service; therefore co-pay would not apply."
And finally there were the clients. Even if they were literate enough to negotiate the brochures and forms sent to them by DSS (the average public-aid recipient has less than a high-school education, and 10-30 percent are illiterate), some of the information, including what phone number to call, was wrong anyway.
In addition, Paulson, of the state workers' union, says that there was little increase in staffing when the changes in Medicaid took effect, and the increased workload -- in combination with inadequate training -- scared many caseworkers away from the job. "Turnover now is extremely high," she says, "so what you're seeing is workers coming into these positions who don't have past experience. You're also seeing supervisors who are unable to supervise multiple programs, because they can't possibly understand all of the multiple changes in all of the programs. Once you have a new worker there, it's trial by fire.
"That's when you find delinquencies and cases that go uncovered because of vacancies," Paulson continues. "Then those get assigned to another worker who has no chance of ever getting on top of that workload. It's overwhelming just to think about."
Because new caseworkers earn little more than $21,000 a year, turnover is extremely high -- 30 percent, by some estimates. "The stress is so high and the pay is so low, they've really had to lower their standards on who they hire," the caseworker says. "You've got people here now with a GED and five years' experience at Taco Bell under their belt."
Another caseworker who asked not to be identified says this: "I have a client with terminal cancer who just signed up for Medicaid. I hate to say this, but I know he won't get his Medicaid before he dies."
Among Missouri's state departments, DSS is a giant. If the state's total expenditures of state and federal money were laid out on a pie chart, "human services," which includes DSS, would take up almost half. DSS spends about $4.8 billion a year to pay for everything from inspecting daycare centers to managing welfare to eradicating juvenile crime. Within DSS are 10,000 employees who are spread out over five different departments including the Division of Family Services (DFS).
DFS in turn operates seven area offices and 114 county offices, which oversee a dizzying array of children's-services programs, rehabilitation services, energy assistance, child-support enforcement, early-childhood initiatives, income-maintenance programs and Medicaid.
When Congress passed welfare reform and subsequent Medicaid-expansion laws, DFS won the prize of figuring out how to do it. Moving welfare recipients off the rolls proved doable. It had to be: Federal mandates required that the state move 50 percent of all single-parent households and 90 percent of two-parent families off welfare by 2002 or lose federal money. Last year, DFS claimed success when it reduced its welfare load by 134,520 people, or 51 percent. Expanding Medicaid, though, posed a different challenge. The biggest problem, as the agency saw it, anyway, had less to do with the complicated new eligibility rules than with finding the people who needed health care. Out there, somewhere, were an estimated 91,000 children eligible for the new program, and DFS had to find them.
Denise Cross, director of DFS, laughs hesitatingly when asked about the task her agency faced in expanding Medicaid. With $52 million in new federal money and $20 million in new state money, DSS created pamphlets, fliers and mass mailings. A phone center was established, computers were reconfigured and a Web page was designed. "We knew we'd have to be more creative and work more effectively with what I would call "nontraditional partnerships' to get word out to families that these programs were available," Cross says. "We already work with social-service agencies, but we felt we needed to broaden out, because there were more children out there we wanted to reach."
The "nontraditional partnerships" included asking providers, hospitals and health-care clinics to pass out information and applications. Parochial schools were asked to send out mass mailings, the agency's Web page listed information, and the toll-free hotline took some 96,000 calls last year. More than 700,000 applications were sent out.
"We've seen an increase of more than 77,000 children since July of '98," Cross says. "That's across all programs, and I don't want to get into all the categories of programs, but the fact is, 77,000 children who did not have health care now do."
But the scramble to get new people signed up, combined with the scramble to get people off welfare, inadvertently led to thousands' being improperly dropped from Medicaid, even though they were still eligible.
Here, in short, is why: Before welfare-reform laws were passed, Medicaid was automatically given to people who qualified for public-aid cash grants. The eligibility for both was determined on the same form, with the same income criteria, at the same time. After welfare reform, which limited the amount of time a person could receive food stamps and cash benefits to five years, the laws required the states to continue Medicaid coverage to ensure that the families wouldn't lose health care at the same time. It was called "transitional Medicaid."
The fear was that welfare-to-work would mean welfare-to-work-that-provided-no-health-insurance, so Medicaid was "de-linked" from welfare and was supposed to continue covering families for 12 months after they left the public-aid rolls. In fact, even if individuals didn't qualify for cash assistance -- either because they got a job or their time limit ran out -- they could still apply for transitional Medicaid. Welfare reform was supposed to ease former public-aid recipients into self-sufficiency, not increase the number of people without health insurance.
The expectation was that since most of the people leaving welfare would not get jobs that provided health insurance, the number of people getting transitional Medicaid would increase proportionately with the number of people leaving welfare.
But that didn't happen.
Joe Squillace, health policy analyst for Citizens for Missouri's Children, says that because caseworkers were broadsided by a torrent of new rules, they didn't understand that when their clients left welfare, they were probably eligible for transitional Medicaid. "The caseworkers were dealing with tremendous caseloads," Squillace says. "They were not informing families or educating them about the availability of Medicaid. Since 1996, there are a lot of children who have fallen through the cracks."
A recent study conducted by Squillace's group shows that at the same time 24,571 children were dropped from the welfare rolls in 1997-98, only 11,772 children were added to Medicaid. In the city of St. Louis alone, the group estimates, 3,533 children who were still eligible for Medicaid were cut off.
Another study conducted by the University of Missouri Department of Economics estimates that of the qualified children whose families left welfare in Missouri from 1997-98, only 38 percent continued their Medicaid coverage.
Still another survey, conducted by DFS, showed that 89 percent of people who were improperly disenrolled from Medicaid when they left welfare said that their caseworkers never told them they might still be eligible for the health-care assistance.
At the Reform Organization for Welfare (ROWEL) in St. Louis, calls from bewildered clients increased 10-fold after welfare reform and Medicaid expansion took hold. Complexity, it seems, had DFS caseworkers by the throat.
"We've had so many complaints from people who've lost their Medicaid, and a lot of the time it's because of what the caseworker didn't know," says Jeanette Mott Oxford, ROWEL's executive director. "I think it is a combination of not being trained adequately and then just the sheer volume of paperwork compared to understaffing."
According to DFS, it had 1,728 caseworkers and added 42 more statewide when Medicaid expanded. Last year, the agency did not request any new hires.
But DFS director Cross refuses to acknowledge that when it comes to caseworkers, the agency is understaffed or that the caseloads are too high.
Asked whether DFS is adequately staffed to run the program, Cross deflects the question and talks about "outreach."
"I really feel that it can't just be done by DFS," she says. "The education, the outreach and the encouraging of folks to come in really has to happen across the community. That's why we've tried to work with folks in the community who have contact with the families.
"I feel that our role is certainly to determine the eligibility and make sure that we get the information out to folks," Cross adds, "but we need the community's help in that."
But are there enough caseworkers to do the job properly?
"I believe that we have implemented the program and we are currently running the health-care program for low-income families," Cross says.
In this mess, Missouri was never alone. In fact, so many states had similar problems with Medicaid expansion that the Clinton administration urged the blanket re-enrollment of the families who had been illegally cut off. Three states have complied so far, and health-advocacy groups in Missouri are calling on DFS to do the same.
"Missouri advocacy groups and the state have acknowledged a systemic problem in terminating Medicaid coverage of families under the guise of welfare reform," says Joel Ferber, an attorney for ROWEL. "These families have not been legally terminated from Medicaid and are therefore still eligible. Consequently, the state is obligated to reinstate them."
The agency concedes that mistakes were made and is in the process of mopping up. But, as some have said, there's a lot to mop up.
"We've done a mass mailing to every food-stamp household whose children do not have health care through any of our programs," Cross says. "We also did a mass mailing to all of the households receiving child-care benefits. We recently did a mass mailing to any children who lost eligibility at any point since November of 1998 to let them all know that health care may still be available to them and sent them applications to reapply."
But advocacy groups aren't convinced that the problems will be fixed.
"Even though we have seen an improvement in the past few months, most of the kids who fell through before are still uninsured," Squillace says. "Those kids should never have lost their Medicaid."
The consequences of welfare reform and Medicaid expansion seem to have had the opposite outcome of what Congress intended. According to the Center for Budget and Policy Priorities in Washington, D.C., more than 1 million fewer children are enrolled in Medicaid than there were before welfare reform.
"Every year more kids are eligible for Medicaid, and every year there are fewer kids enrolled," says Elizabeth Schott, senior policy analyst for the Center. "There's been a 50 percent decrease in the number of (welfare) cases nationally, and most of those people should have been eligible for Medicaid. But studies from the states indicate that only about one-third of the adults and only half of the children are getting Medicaid coverage.
"There's clearly something very wrong," says Schott. "And it doesn't have to be that complicated. If anything, the new laws have created the potential for things to be much simpler. I don't know if the states that are saying this is too complicated, don't understand or are choosing not to understand."
Schott points to the District of Columbia, where all children in all families with incomes up to 200 percent of the poverty level are covered. Period. Few questions asked. "It's easy," Schott says. "There's nothing complicated about it. I think that the states are unwilling to spend the resources and are sort of hiding behind complaints of complexity when they could make it very simple."
Goldstein, the social worker, agrees.
"In Missouri, they're boasting that they're covering families up to 300 percent of the poverty level, but in reality they're not," she says. "With Fayzen Woods, for example, it took me, a social worker with 20 years of experience; my co-worker, who is a lawyer; and two program specialists in the state office to get her into a better package of benefits. How many people do you think get that kind of help?
"If they say they're going to cover people up to 300 percent, then cover people to 300 percent -- parents, children, everyone. Same benefits. End of story. None of this some-of-it-is-covered, some-of-it-is-not stuff. It wreaks havoc," Goldstein continues. "Maybe it would have been better to just raise it to 200 percent and have a better program at least, and then go from there. It is a joke now. It's almost impossible."
In July 1999, DSS began formally training its caseworkers on the new system and about how to ensure that everyone who qualifies for Medicaid receives it. Even with the training, though, many caseworkers still say they feel overwhelmed.
At the federal level, the Clinton administration's budget for 2001 calls for $2.7 billion to increase the number of uninsured children in CHIP. Part of the money will go toward making enrollment in Medicaid easier to understand.
But advocacy groups such as ROWEL say they want a full-fledged assault on the problem. In addition to reinstating any welfare family cut off from Medicaid, they want ongoing monitoring, more supervisory review, ongoing training for caseworkers and notices that the clients understand. If, for instance, a client leaves welfare, he or she should receive a notice that simply says, "YOU ARE STILL ELIGIBLE FOR MEDICAID!"
"They've been trying to fix some of the problems," says Mott Oxford of ROWEL, "but there are a lot of problems to fix."
Several days after the beginning of the new year, Fayzen Woods enlists the help of her three children to scour, top to bottom, the apartment they've lived in for the past seven years. It is a twice-a-year event, this family "spring cleaning," and the kids can be heard upstairs pulling everything out of their closets. The apartment, still sparsely clad in Christmas decorations, smells like bleach.
At one point, rap music from Woods' oldest son's radio thumps down through the ceiling, and Woods, creases forming on her brow, slips away from the conversation taking place at the kitchen table. The music suddenly stops, and Woods reappears at the table.
"Sorry about that," she says.
"No problem," says Goldstein, who is here to make sure Woods understands the ins and outs of her new Medicaid coverage. It has been five months since Woods first called Goldstein's office, and though she's back at work driving a school bus now, she's still trying to catch up on all the bills. Buying Christmas presents this year didn't help.
It also didn't help that Woods lost her cash-grant eligibility. Several weeks after losing her EBT bank card, Woods was asked to come into the DFS office for a meeting with her caseworker. She didn't know why.
She went at 9 a.m. but was told the caseworker couldn't see her yet. By 10 a.m. the caseworker was still not available and Woods started to worry, because she had a noon appointment to see about getting a student loan. By 11:30 a.m., the caseworker was still unavailable, so Woods left for her second appointment. One month later, she was notified that her cash grant was being cut off -- because DFS couldn't verify her income because she never met with her caseworker.
"Remember that information you sent me about your insurance?" Goldstein asks. "I said I think we can get you into MAF, which is a better category, because it isn't time-limited. But when you went back to work, your income automatically put you into transitional Medicaid and your kids into Medicaid for Kids, which is called MC+ just to confuse us."
Woods nods her head as if she understands: "So I'm on a timed thing?"
"No you're not. Transitional Medicaid you can only have for 12 months, but this new rule says that if somebody is on TANF and MAF and they get a job...."
"What is TANF?"
"That's the cash grant."
"And MAF?"
"That's the Medicaid that is connected to TANF. But you don't have to get the TANF to get the MAF. But you have to meet the same criteria for income."
"This is hard stuff," Woods finally admits.